
Hemmel Amrania developed Digistain’s infrared spectrometer.Credit: Chris Ratcliffe for Springer Nature
In the corner of a physics laboratory at Imperial College London sits an unassuming white box not much larger than a kitchen stand mixer. Although its physical footprint is small, its impact on cancer care could be huge. This is the prototype of Digistain’s infrared spectrometer, an instrument that allows clinicians to extract biochemical information from tumour samples and decide what treatment to give people quickly and at a fraction of the cost of existing technologies.
Its creator, Hemmel Amrania, enthusiastically demonstrates how it works. A pathologist begins by preparing a sample of a tumour as they usually would: fixing the tissue with formaldehyde, embedding it in wax and cutting it into thin slices. The next step would typically be to stain the slices with dyes and examine them under a microscope. But by adding a simple step — sliding an unstained slice into the spectrometer — the pathologist can capture thousands of data points about the molecules in the tumour cells faster, with greater precision and at a much lower cost than before.

Hemmel Amrania uses liquid nitrogen to cool down the detector of the spectrometer to allow signals from tumour tissue to be recorded.Credit: Chris Ratcliffe for Springer Nature
Infrared spectroscopy relies on the fact that different molecules absorb different wavelengths of infrared light. By shining infrared light on a sample and analysing the wavelengths that are absorbed, scientists can deduce the concentrations of specific molecules in it. Although spectrometry has been used by chemists for decades, it is only with advances in the machine’s detectors that the technology is now sufficiently sensitive and cost-effective to apply to oncology.
The seeds of Digistain’s creation were sown in London’s Charing Cross Hospital. Amrania, then a physics PhD student at Imperial, was investigating possible biological applications for light spectroscopy. He got talking to some oncologists at the hospital who were using tumour biopsies to help them to decide which of their patients could avoid chemotherapy. To Amrania’s surprise, the oncologists were sending samples to California for expensive and time-consuming molecular testing. “What I noticed”, he says, “was there was an opportunity to make a bigger impact, both with the patients and with the clinical pathway, if we were to deliver a test result far more quickly but also far more accessibly.”
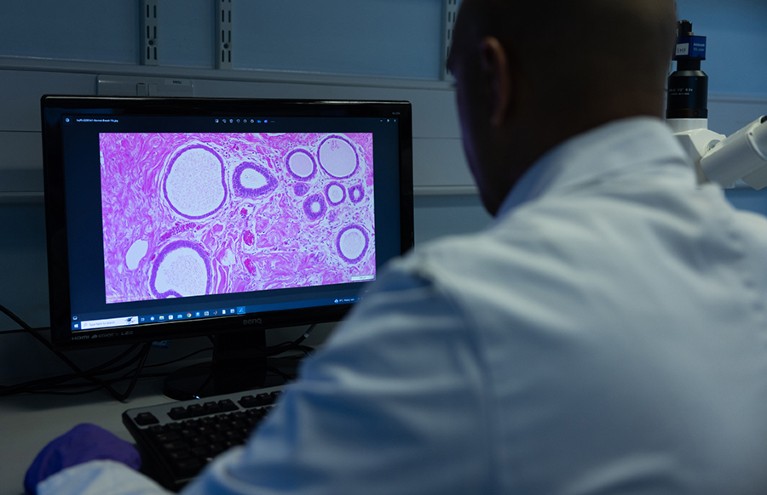
Stained tumour tissue is examined for irregularities.Credit: Chris Ratcliffe for Springer Nature
The decision about who should have chemotherapy after a tumour has been removed, known as adjuvant chemotherapy, can be fraught. If prescribed appropriately, this procedure can prevent tumour recurrence. But chemotherapy comes with a range of unpleasant side effects that can have a severe impact on a person’s quality of life.
“The main challenge in cancer is to do no harm,” says Anand Sharma, a clinical oncologist at Mount Vernon Cancer Centre in Northwood, UK, which is using Digistain and is part of the country’s National Health Service (NHS). The ability to identify who is at high risk of relapse will prevent others receiving chemotherapy unnecessarily, he says. “Digistain helps in overcoming this hurdle, because we are able to identify patients who are at risk of relapse and tailor treatment accordingly.”
Curbing chemotherapy
For the past 50 years, oncologists have relied on microscopic studies of a person’s excised tumour to guide the use of adjuvant chemotherapy. Pathologists study stained slices of tumour to assess the appearance of the cells and arrive at a ‘grade’ that helps them to indicate how aggressive a tumour is. A tumour’s grade can be combined with other factors to come up with a numerical score to aid prognosis. A commonly used formula in breast cancer, for example, is the Nottingham Prognostic Index, which takes into account the grade as well as the size of the primary tumour and the number of lymph nodes that contain cancer cells.

Hemmel Amrania (left) and the Digistain team.Credit: Chris Ratcliffe for Springer Nature
But grading is an imperfect tool: it relies on the subjective judgement of individual pathologists and the results can vary depending on which part of the tumour is sampled. “The original inspiration for Digistain came from trying to eliminate the subjectivity in tumour grading,” says Amrania. The physical appearance of cells under a microscope can sometimes be misleading. Cells that look physically similar can have distinct faults with their molecular wiring, and so behave very differently.
For some cancers, such as certain kinds of early-stage breast cancer, this means it can be hard for clinicians to predict who will need adjuvant treatment. So, for many years, physicians erred on the side of caution and prescribed chemotherapy to those who might not have needed it.
The early 2000s brought improvements in the form of tests that probe the molecular make-up of tumour samples, for example by looking at the activity of particular sets of genes associated with tumour prognosis. For certain types of breast cancer, these tests include Oncotype DX and MammaPrint1. Both of these profile the activity of genes relating to tumour-cell proliferation, an indicator of how aggressive a tumour is.
Although such tests have been transformative, they have drawbacks. They are complex to administer, requiring samples to be sent away to specialist laboratories. Results can take several weeks, especially if the samples are being sent internationally. What’s more, their high cost (US$3,000–4,000 each) limits their use to those who are deemed eligible (about half of people with early-stage breast cancer), either by public health-care systems or by private health insurers.
Attacking aneuploidy
To address these challenges, Amrania teamed up with his colleagues at Imperial. Physicist Chris Phillips, medical oncologist Charles Coombes, and the late histopathologist Sami Shousha, as well as histopathologist Nicholas Wright at Barts Cancer Institute in London, decided to use infrared spectroscopy to look for the presence of abnormal numbers of chromosomes, or aneuploidy, in breast tumour cells. Aneuploidy results in enlarged cell nuclei and is characteristic of cancers that are more aggressive, are prone to drug resistance and have a poorer prognosis. It also reflects tumour cell proliferation. “This is a very robust and independent prognostic marker for breast cancer,” says Amrania. “It’s just very difficult to measure” using the conventional tool of laser flow cytometry, he adds.
Digistain’s technology involves using infrared spectroscopy to assess the ratio of DNA to protein at a particular point in the tumour slice. This ratio reflects the size of the cell’s nucleus in relation to its cytoplasm, and hence its degree of aneuploidy. The company’s software then calculates a number — dubbed the Digistain Index — that reflects the nucleus-to-cytoplasm ratio and therefore the level of aneuploidy in the tumour. In 2018, the company published the results of a trial in which its scientists compared Digistain assessments of breast-cancer samples against conventional grading performed by pathologists2. This showed that the correlation was “extremely high”, says Amrania.
The next step was to see whether incorporating the Digistain Index with other clinical factors could predict the risk of recurrence. So the team performed a study3 on a cohort of 801 women with a specific type of early-stage breast cancer. The analysis combined the Digistain Index of biopsies with a number of other factors — age at diagnosis, the presence of cancer cells in nearby lymph nodes, tumour grade and tumour size — to yield the Digistain Prognostic Score that classified people as being at either high or low risk of tumour recurrence. Comparing this grouping against the known outcomes of the people in the test group showed that the Digistain Prognostic Score was at least as reliable as existing risk-stratification tests. The Digistain Prognostic Score is now being used instead of the Nottingham Prognostic Index in some clinics.
Digistain’s lower cost and rapid turnaround time sets it apart from its molecular-test competitors. It does not require expensive reagents, meaning that the company can bring the price down to roughly 25% of that of molecular tests. What’s more, the spectroscopy equipment is similar in cost to a standard pathologist’s microscope, and the tests can be run by junior staff. “We’re enabling the NHS to perform these tests in their own pathology labs for the first time,” Amrania says. According to an economic analysis by the consultancy Health Tech Enterprise in Cambridge, UK, in January, swapping the incumbent technology for Digistain for breast cancer would save the NHS £287 million (US$365 million), without increased risk to patients. Digistain is planning to publish the results.
Digistain is now preparing clinical trials for lung, colon and kidney cancer. For kidney cancer, in particular, there are few molecular tests available to support clinicians. “That means quite a significant number of patients will be getting adjuvant treatment,” says Sharma. The trial was approved by the UK National Institute for Health and Care Research in October 2023, and will involve 17 centres across the United Kingdom, with Sharma at the helm.
Digistain also aims to broaden its impact beyond the United Kingdom. The technology is particularly appealing in low- and middle-income countries. Digistain is already in routine clinical use in India, the Philippines and Ecuador. In the United Kingdom, meanwhile, the private medical insurance company Bupa has not only agreed to reimburse Digistain testing, but also amended its clinical guidelines to prioritize the use of Digistain in clinical decision-making in breast cancer. In 2023, the NHS inducted Digistain into its Innovation Accelerator, which helps new technologies to be adopted faster and more systematically in the NHS. Digistain is already working with several NHS centres around the United Kingdom.
It’s a far cry from the physics lab in which Amrania began his work. But Digistain is a testament to the power of moving research out of its conventional silos. “As scientists,” Amrania says, “we stay in our lanes far too often.”
