People travel from across South Korea to receive medical treatment in Seoul.Credit: Will & Deni McIntyre/Getty
Later this year, South Korea is expected to sign up to the European Union’s research-funding programme, Horizon Europe. It’s a good time to reflect on the nature of large collaborative projects — and, in particular, when cross-border collaboration is most beneficial and when a deeper dive into local issues can be more rewarding.
Large international collaborations have unquestionably produced great breakthroughs. Sequencing the human genome, for example, took 13 years of work by 20 institutions in 6 countries1. But large consortia such as these are almost always established in the same few countries: the United States, the United Kingdom and others in Europe. For scientists working elsewhere, setting up a large international project can seem unachievable, given the billion-dollar price tags and the networks of contacts required.
And, sometimes, it is not the best solution. Global projects spearheaded in a few countries can have biases — for example, people of Asian descent are often under-represented in international genetic studies initiated in the West. National laws on acquiring data can differ, meaning that researchers need to conduct experiments differently in different regions, introducing biases. And the logistical complexity of coordinating a project across multiple countries in different time zones and with different work cultures can be problematic when rapid data collection and analysis are crucial2.
There is an alternative — set up a large local consortium in one nation.
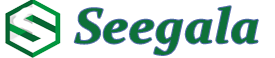
Cancer research needs a better map
We’ve done just that in Seoul. Our single-cell atlas of immune diseases (SCAID) consortium is a multi-institutional effort led by one of us (J.-I.K.), alongside 23 others. Running since April 2022, the project now involves 120 South Korean clinicians, immunologists, geneticists and bioinformaticians (including S.L., H.L. and J.K., who work in J.-I.K’s group).
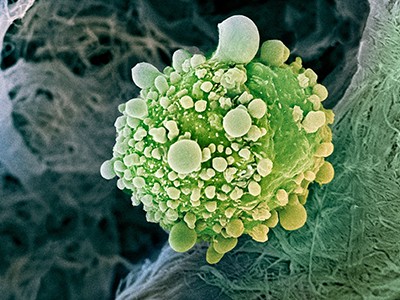
We aim to map gene expression in millions of individual cells from people who have immune-related diseases , including (but not limited to) rheumatoid arthritis, inflammatory bowel disease, interstitial lung disease and alopecia areata. Systemic immune diseases are thought to affect at least 1 in 20 people3. They are often incurable and cause debilitating symptoms, from chronic skin rashes to skeletomuscular changes. They can be fatal if they are not managed appropriately. We hope that our research will reveal similarities between 16 diverse diseases that manifest across the body, and help to uncover ways to use treatments more effectively.
Our experiences have shown us that a regional consortium can be an efficient way to ask crucial research questions. Here, we share two broad lessons that we hope will help others to build effective regional consortia.
Find a niche
To compete in international circles, local consortia need to focus on addressing research questions that they are in a unique position to answer. This might be because of the particular mix of expertise of local researchers. It might be the regulatory environment in a country. Or it might be specific to the geography of the place where the research is done.
In our case, we were inspired to set up SCAID by an international consortium called the Human Cell Atlas (HCA). Since 2016, it has been trying to map every single cell type in the human body using state-of-the art genomic technology. The next logical step is to create similar atlases for diseased cells. But this involves bringing in specialized clinicians for each disease and obtaining proper consent from a large number of people.
This can be hard to achieve in a global consortium, in which each country has distinct legislative frameworks, ethics committees and medical systems4. For instance, the International HapMap Project — a genome-sequencing project launched in 2002 with researchers from six countries — needed to spend months in community consultation in Nigeria before it was able to obtain ethics approvals5. It also faced concerns raised by community advisory groups in Japan and China around depositing biological samples in overseas repositories. Overcoming these obstacles took 18 months6.
For these reasons, most single-cell studies of disease data sets have focused on single diseases in single tissues, for simplicity. By contrast, restricting our study to a single country with one legislative framework has made it easier for us to gain ethics and individual approval, allowing us to study multiple diseases across multiple tissues.

Seoul National University Hospital is one of 56 general hospitals in the South Korean capital.Credit: Anthony Wallace/AFP via Getty
Seoul also has other benefits for such a project. First, it’s easy to enlist a diverse range of participants in the city. South Korea has a universal medical-insurance system that is mandatory for all residents7. This avoids biases that can arise when participants are part of a private health-insurance system. And people from across the country and all socio-economic classes travel to Seoul for treatment — the city’s cluster of 56 general hospitals can be reached from anywhere in South Korea in half a day.
The concentration of hospitals also makes it easy to transfer samples quickly from donors to our central laboratory for analysis — it is no more than two hours’ drive from any hospital. Such proximity is a great advantage in single-cell genomics, because RNA — which is analysed to ascertain gene expression — degrades within hours once a sample is collected. A US National Institutes of Health large-scale genetics project called the Genotype–Tissue Expression project, for instance, found variability in the quality of RNA in its samples, depending on the time between collection and processing. This variability could skew interpretations of gene-expression data, and the researchers had to develop ways to account for it in their analyses8.
Having a centralized hub prevents the problem of batch effects — undesired differences between samples — that can arise if samples are processed or analysed differently by different centres9,10. Handling batch effects is a big task for international consortia. The HCA, for instance, has a dedicated team of researchers to check for and minimize such effects11.
Exploiting this niche is already proving fruitful for us. So far, we’ve collected more than 500 samples from 334 donors. We have analysed more than two million cells — equivalent to the second-largest data set collected in the HCA project so far. Our early analysis hints at common features between diseases: although symptoms arise in different organs, we are identifying distinct immune profiles that group the diseases into a few major categories.
Unblock research bottlenecks with non-profit start-ups
Still, being small and nimble comes with challenges. Local consortia need to be aware that they might lack some expertise, and they need to be prepared to seek help. Our consortium faced obstacles in obtaining ethics approvals, because each hospital review board had different requirements and concerns. Getting approval from each board was arduous, and required persistence when asking for opinions of the boards themselves, along with those of the Korea National Institute for Bioethics Policy and Korean Bioinformation Center. Nonetheless, it was easier than grappling with multiple international rules around ethics and data collection.
To make this process smoother for others, it would help for institutions in a country to standardize their ethical-review processes and data-sharing agreements, ensuring that both comply with national regulations. Furthermore, institutions should establish collaborative networks to share best practices and discuss common challenges. These steps could ease the administrative burden on local consortia considerably, and accelerate their progress.
Not all countries will have the strong technical skills of the South Korean workforce, nor the established biobanking repositories for genetic and clinical data, which are essential in projects such as ours. For scientists in countries without this infrastructure, international consortia can be a valuable source of guidance. For instance, the HCA’s Equity Working Group specifically aims to engage diverse geographical and ethnic groups in its projects12. By participating in such initiatives, countries can gain access to expertise, resources and best practices, helping them to overcome technical challenges and build their capabilities.
Build in local benefits
Regional projects should reflect the needs of the local community, both for ethical reasons and to attract funding. Funders are more likely to invest in big projects that can benefit citizens. Researchers must make those benefits clear.
This might mean championing a field to governments and other funders. In South Korea, most research funding comes from the government — scientists propose broad topics that need funding, and the government selects those that align with its own goals and puts out funding calls, for which all researchers can apply. So genomicists, immunologists and bioinformaticians — not all of whom are members of the SCAID consortium — requested that the South Korean government fund a large-scale disease single-cell atlas. These scientists spelled out how the data could ultimately help researchers and clinicians to improve understanding of the disease predispositions that are unique to South Koreans. This will hopefully speed up the development of precision medicines tailored to the country’s own population.
South Korean scientists’ outcry over planned R&D budget cuts
In countries that do not have official channels for petitioning the government, raising the profile of a field might involve using networks of contacts to meet with funders, or publishing papers that outline a field’s potential. Persistence is key — scientists must keep voicing their needs and perspectives.
Researchers must also give careful thought to how their project will benefit local science. SCAID was designed to maximize the long-term benefits for the South Korean researchers and clinicians involved.
To develop researchers’ careers, we hold regular seminars and workshops focused on learning skills and network building. Cross-disciplinary collaborations are one focus. For example, bioinformaticians are working with clinicians on a strategy pinpointing the specialized data that should be collected for each disease — such as acquiring information on immune receptors for specific disorders. Bioinformaticians are also exploiting the expertise of clinicians to help interpret their analyses. This includes the identification of abnormal cell states, which can be hard to distinguish from artefacts in the data without a deep knowledge of disease. These networks of contacts will be useful for many projects long after SCAID is completed.
What next?
Once established, local consortia need not exist in isolation. They can complement existing global projects by adding diverse data, and can act as stepping stones for future global consortia. For instance, many scientists have approached us, intrigued by the scale and potential of our work, and enquired about possible collaborations.
We are keen for other regional groups to generate international databases from separate efforts led by those who understand their own local needs and niches best. We encourage them to start by seeking funding for a consortium to address the needs of their fellow citizens, and to eventually pool their knowledge.
Whatever the field, if a consortium is run well, it can cultivate a dynamic cluster of competent researchers, laying the groundwork for international recognition and collaboration.