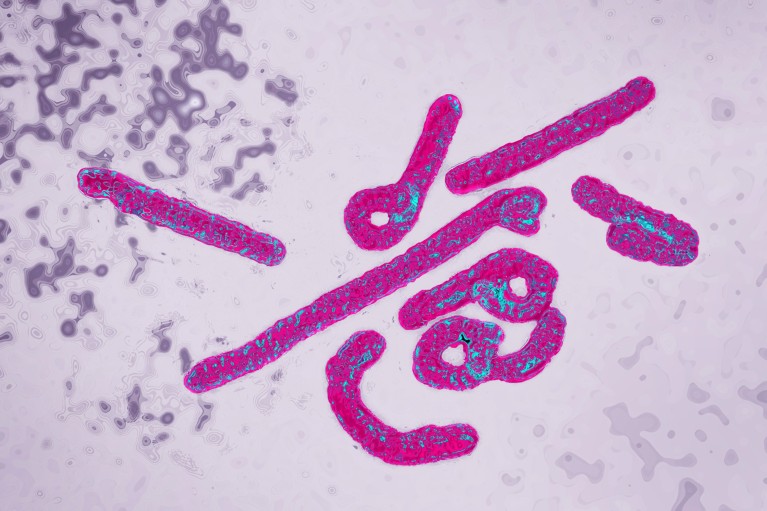
Marburg virus (artificially coloured) is related to Ebola virus and causes similar symptoms.Credit: James Cavallini/Science Photo Library
It is an outbreak of superlatives. One of the deadliest known viruses, Marburg, has emerged in Rwanda, killing 13 people and sickening 58 in one of the biggest Marburg outbreaks ever documented. Scientists expect the outbreak to be curtailed quickly — but they warn that, overall, Marburg is on the rise.
The outbreak, which was declared on 27 September, is Rwanda’s first. Tanzania and Equatorial Guinea recorded their first Marburg outbreaks last year; Ghana’s first was in 2022. Before the 2020s, outbreaks were detected at most a few times each decade; they now occur roughly once a year. The origins of the events are not entirely clear. But researchers say that environmental threats, such as climate change and deforestation, have made people more likely to encounter animals that can pass on infections.
Outbreaks of animal-transmitted diseases are “going to continue to become more frequent”, says emergency-medicine physician Adam Levine at Brown University in Providence, Rhode Island. “The world really has to just be ready for that.”
Ebola’s close relative
Marburg virus is a “cousin” to Ebola virus, which killed more than 11,000 people during an outbreak in West Africa between 2014 and 2016, says virologist Adam Hume at Boston University in Massachusetts. The death rate from Marburg has ranged from 23% to roughly 90% in past outbreaks. There are no vaccines or treatments, but supportive care increases a person’s odds of survival.
Early Marburg symptoms — high fever, headache and malaise — are similar to those of many other diseases. But people with Marburg soon develop severe diarrhea, nausea and vomiting. The worst afflicted bleed from their noses, gums or other areas.
After the genocide: what scientists are learning from Rwanda
In Rwanda, some of the first people later found to be infected with Marburg initially tested positive for malaria. Health-care workers knew something was amiss when the usual treatment wasn’t working. By the time the workers realized they had a Marburg outbreak on their hands, a number of them had already become infected, Rwandan Minister of Health Sabin Nsanzimana said in a press conference last week.
The outbreak is weighing on the minds of Kigali residents, says Olivia Uwishema, Rwandan-born founder of Oli Health Magazine Organization, a non-profit group in KIgali. Uwishema lives in the United States but happened to be visiting Kigali when Marburg hit. Now when someone gets a fever, “they mostly think that it may be Marburg”, Uwishema says.
Stopping the spread
The good news is that Marburg is transmitted mostly through contact with bodily fluids. That means that isolating infected people and using protective equipment can deter spread effectively, Levine says.
For the next three weeks, contact tracers in Rwanda will be checking in with hundreds of people who were in direct or indirect contact with individuals with Marburg. Health-care workers are testing everyone who presents with a high fever for the disease. This has put a strain on the country’s diagnostic laboratories, given the prevalence of malaria.
Rwanda’s widespread testing for the virus might account for the current outbreak’s large size. Many past outbreaks were reported to have affected only a few people, Uwishema says. But cases might have been missed in countries whose health-care systems are not strong enough to offer the level of testing that Rwanda has achieved.
The outbreak can be declared over if no new infections arise for 42 days — equivalent to two incubation periods for the virus — after the last case is identified. “In the coming weeks, we should have a good sense about whether it is rapidly growing or rather petering out,” Levine says.
Vaccine testing underway
Marburg outbreaks usually start after a person encounters an infected fruit bat — an animal that can carry the virus without getting sick. Because of forces such as climate change and deforestation, “boundaries between the wildlife and the humans are breaking down”, creating ever more frequent opportunities for pathogens to jump to people, said global-health expert Caroline Ryan at Ireland’s Department of Agriculture, Food and the Marine in Celbridge.
Meet the Ebola workers battling a virus in a war zone
Vaccines and drugs could help to curb Marburg, but to test these tools thoroughly, scientists must wait for outbreaks to happen. “That’s one of the reasons why, I think, we don’t have therapeutics and vaccines that are approved against Marburg virus,” Hume says.
Rwandan doctors have started testing a candidate Marburg vaccine, and plan to test the efficacy of the antiviral drug remdesivir against the disease. Animal trials1 suggest that remdesivir might be helpful for treating Marburg, as it is for COVID-19. But data from human trials investigating remdesivir as an Ebola therapy “were a little disappointing”, Hume says, raising the prospect that the drug won’t be useful for Marburg either.
However, the identification of effective antiviral will not be enough, health officials say. To weather future outbreaks, Africa must build its capacity to manufacture vaccines, treatments and diagnostic tools on its own, said Jean Kaseya, director-general of the Africa Centres for Disease Control and Prevention, last week. Relying on other countries to sell such supplies at high prices can lead to “panic mode”, he said.