Tecovirimat, an antiviral drug, has been used to treat mpox.Credit: Elijah Nouvelage/Bloomberg/Getty
The drug tecovirimat did not accelerate healing for people in a clinical trial in the Democratic Republic of the Congo (DRC) who were infected with a concerning strain of the monkeypox virus, according to the US National Institutes of Health (NIH). The strain, called clade I, has been spreading across Africa and is thought to be more lethal than the one that caused a global mpox outbreak that began in 2022, known as clade II.
Growing mpox outbreak prompts WHO to declare global health emergency
Tecovirimat, an antiviral, is commonly used to treat mpox, despite limited clinical evidence that it resolves symptoms. The drug was originally developed to treat smallpox, which is caused by a related orthopoxvirus.
“These are certainly not the ideal results that we were all hoping for,” says Jason Kindrachuck, a virologist at the University of Manitoba in Winnipeg, Canada.
Clade I’s spread in the DRC and other countries in Africa prompted the World Health Organization (WHO) to declare a public health emergency of international concern on 14 August — its highest level of alarm. A day earlier, the Africa Centres for Disease Control and Prevention (Africa CDC) declared its first-ever public-health emergency over the outbreak.
And yesterday, Sweden reported its first case of a person infected with a variant of clade I, called clade Ib, that scientists reported in April as being able to spread among people through sexual contact. Prior to last year, clade I was thought to transmit through household contact and through contact with infected wild animals.
Disappointing results
During the trial, launched by the NIH’s National Institute of Allergy and Infectious Diseases (NIAID) and the DRC’s National Institute of Biomedical Research, people infected with clade I were given either tecovirimat or a placebo pill. According to the NIH, which announced early results on 15 August, the antiviral did not reduce the duration of mpox symptoms compared with placebo.
Can a smallpox drug treat monkeypox? Here’s what scientists know
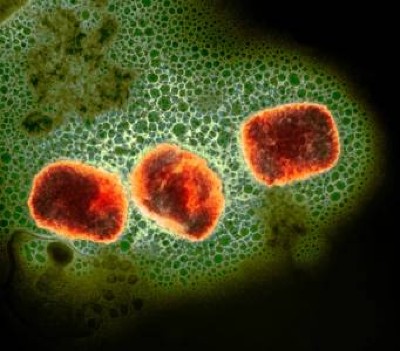
Mpox, the disease caused by the monkeypox virus, can cause fluid-filled lesions, fever, headache and, in severe cases, death.
Significantly, however, the study participants’ mortality rate, regardless of whether they received tecovirimat or placebo, was lower than the overall mortality rate for any type of mpox typically reported in the DRC: 1.7% versus 3.6%.
This could be because of the care that the participants received during the trial. The 597 people enroled in the trial were hospitalized for at least 14 days, a period in which they received, among other things, nutritional support; proper hydration; treatment of any other infections or diseases they might have, including malaria; and psychosocial support.
“The level of care was very high,” says Lori Dodd, a biostatistician at NIAID in Bethesda, Maryland, and the project leader for the trial. Maintaining that high quality of care outside of a clinical trial could be challenging, she adds, “so the team will be working on how to translate that care model for people with mpox who are recovering on an outpatient basis and in resource-limited settings”.
Hope for specific groups
The maker of tecovirimat, New York City-based SIGA Technologies, suggested in a press release that trial participants who received early treatment with the drug and those with severe disease had a “meaningful improvement”. But the full data have not been released. They are being analysed, and a manuscript is being prepared for submission to a peer-reviewed journal, Dodd says.
“We are all eager to see the paper, in particular to see if there is any group that could be selectively targeted for treatment, especially people with HIV”, says Piero Olliaro, an infectious-disease specialist at the University of Oxford, UK, adding that outcomes for people with advanced HIV and who get infected with the monkeypox virus tend to be worse1.
Monkeypox virus: dangerous strain gains ability to spread through sex, new data suggest
It’s not yet clear whether the trial results can be extrapolated to clade Ib. “We don’t know a lot about clade Ib for the time being, and we need more investigations into the clinical presentation and outcomes to inform whether new clinical trials are required,” Olliaro says.
Although these preliminary results for tecovirimat are disappointing, Kindrachuck says, they do point to the fact that “if we get resources into the DRC and beyond for support for patients with clade I mpox, we can actually increase recovery”.
Nicaise Ndembi, a virologist at Africa CDC who is based in Addis Ababa, says that the results do not change the response plan to the current outbreaks, which includes enhancing surveillance, increasing laboratory testing, strategically distributing the limited vaccine doses available and negotiating the acquisition of additional doses. But he says that they highlight the fact that appropriate standard-of-care is crucial to reduce mortality related to mpox.
Although a vaccine against mpox, made by biotechnology firm Bavarian Nordic in Hellerup, Denmark, exists, it is still largely unavailable in African countries. Bavarian’s chief executive Paul Chaplin, however, reported to STAT News that the European Union has placed an order for 175,000 doses to be donated to Africa CDC.
With additional reporting from Max Kozlov.