By the end of 2023, there were around 43 million refugees globally. But many more — roughly 68 million people — were displaced in their own countries because of armed conflicts and violence1. In 2023 alone, there were 20 million incidents of internal displacement across 45 countries and territories — with Sudan, the Democratic Republic of the Congo (DRC) and Palestinian territories accounting for nearly two-thirds of the total2.
For decades, the problem of internal displacement has been marginalized by governments, United Nations agencies, donors of humanitarian aid and global health researchers. Between 2010 and 2019, international aid for health care for internally displaced people fell from an annual amount of US$5.34 to $3.72 per capita — whereas aid for refugees in low- and middle-income countries increased from $18.55 to $23.31. By 2019, aid for health care per capita for internally displaced people globally was about one-sixth of that for refugees3 (see ‘Decades of neglect’). Likewise, after searching through PubMed, a database of biomedical and life-sciences literature, we found that over the past four decades, about 15–20 times more papers have been published on refugee health than on the health of internally displaced people.
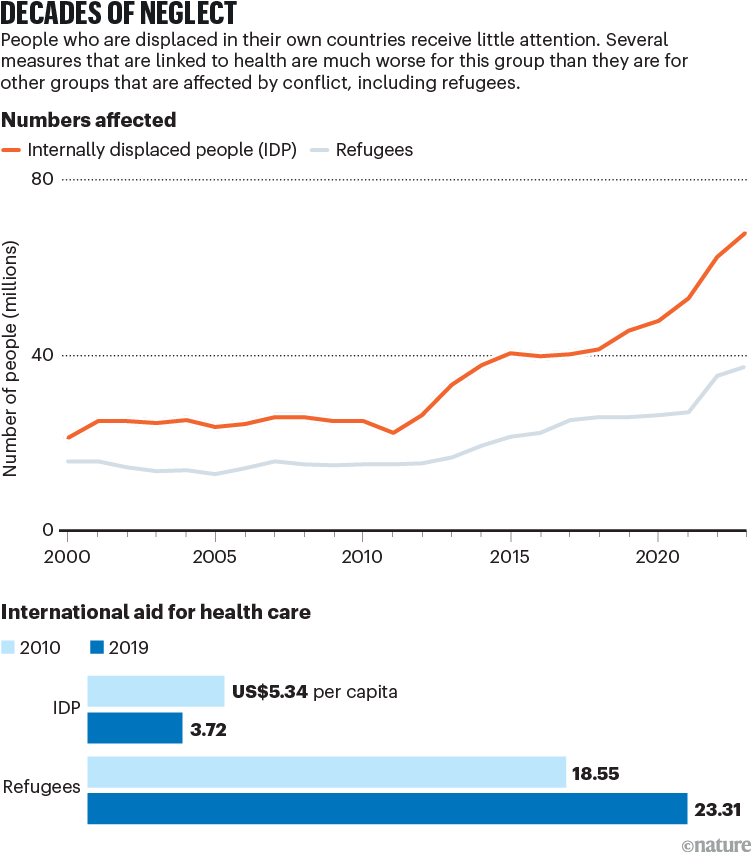
Sources: IDMC; UNHCR; Ref. 3
Several initiatives have begun to address the problem. To lessen severe inequity and prevent epidemics and pandemics, the international community must build on this momentum and ensure that much more attention and resources are directed towards the needs — particularly the health needs —of internally displaced people.
An unseen crisis
Findings from various investigations conducted over the past three decades indicate that in populations that are affected by conflict, numerous measures linked to health are much worse for internally displaced people than for other groups, including refugees.
Studies have shown, for example, that in camps for internally displaced adults and children in Sudan — and among internally displaced people in Myanmar who were not living in camps — mortality rates were well above the rate considered to signal a health emergency4,5 (on the basis of internationally agreed standards). Also, meta-analyses have shown that mortality rates for internally displaced people are consistently higher than for non-displaced people living in the same country. They are also higher than for refugees who have fled that country6.
Internally displaced people are more likely to be affected by disease than are those in other groups — including refugees. A 2016 study of displaced children under the age of five who were living in a camp in the DRC showed that they were more than twice as likely to have malaria than were children of the same age who were living in a nearby village7. Between 2009 and 2016, in Colombia, even internally displaced people who were not living in camps were more prone to infectious diseases than were people who had not been displaced8. A 2021 study collates multiple sources of evidence and indicates that these effects are sustained for multiple diseases and can persist for years or decades and even across generations9.

A health worker gives medicine to a woman displaced by floods in Nigeria.Credit: Olympia De Maismont/AFP via Getty
All sorts of intersecting factors contribute to the disproportionate level of health problems for this population.
Those who are forced to flee their homes because of armed conflict or violence tend to live in relatively poor countries, where fighting has destroyed infrastructure and depleted already struggling health systems. Between 2009 and 2021, 83 countries and territories recorded internal displacement because of conflict and violence. Only one — Israel — was a high-income country10. Also, conflicts often disproportionately affect economically disadvantaged populations and, in many civil wars, displaced people tend to originate from the poorest regions of a country.
Economic and social challenges are drastically worsened after people lose their houses, livelihoods, resources and support systems. Besides dealing with stigma and the suspicions of governments and local communities that internally displaced people might be to blame for conflict, these people often face legal or bureaucratic obstacles when trying to access a place to live, schools and health care. The effects of climate change, extreme weather events and earthquakes often compound the difficulties faced by internally displaced people because they tend to end up living in more precarious locations, and are less able to cope with flooding, landslides or other challenges10.
Why the neglect?
The 1951 Refugee Convention outlines the responsibilities of nations towards individuals who arrive as refugees, and the rights of individuals who are recognized as refugees. Several global health researchers have proposed that a similar treaty should be created for internally displaced people11.
But internally displaced people have the same legal rights, including to health care, as other citizens of their country. Also, the UN’s Guiding Principles on Internal Displacement, the African Union Convention for the Protection and Assistance of Internally Displaced Persons in Africa (also known as the Kampala Convention), and various national laws and policies in many conflict-affected countries already outline the responsibilities of states for this group of people.
In our view, the problem is not a lack of formal legal rights, but inadequate action on the ground — principally from governments and from the international humanitarian community.

Children walk between tents set up for internally displaced people in Gaza City, Gaza.Credit: Mahmoud Issa/Middle East Images/AFP via Getty
Key institutions, such as the World Health Organization (WHO), as yet lack specific policies, plans and guidelines for health care for this group. The WHO’s global action plan on promoting the health of refugees and migrants, for example, barely mentions internally displaced people. So far, this group has received scant attention in the publications and activities associated with the WHO’s Health and Migration Programme — an effort to secure the health rights of refugees and migrants and achieve universal health coverage.
Likewise, little provision is made for the health of internally displaced people across the wider humanitarian system — which includes UN agencies such as the WHO but also international donors, such as the US Agency for International Development (USAID), and humanitarian non-governmental organizations. Too often, the health needs of internally displaced people are treated as if they were the same as those of the general population in that country.
People who leave their country and cross a border present a highly visible and politically charged challenge, which governments are under pressure to address. Internally displaced people lack this visibility. It can also be hard for international agencies and media organizations to gain access to this group of people, because of the violence happening in their countries. Furthermore, governments of countries affected by armed conflict can be resistant to outside involvement, or reluctant to assist internally displaced people, suspecting them of being associated with rebel groups.
Conservation policies must address an overlooked issue: how war affects the environment
Yet, the current situation is untenable. Studies have shown that the main causes of death and ill-health during wars often stem from the indirect effects of armed conflict rather than from the direct violence. In the DRC in 2003–04, for example, for every one person killed by violence, it was estimated that nine people died from easily preventable and treatable illnesses, such as diarrhoea and malnutrition12. Internal displacement is often a major driver of this excess mortality and morbidity.
High levels of mortality and morbidity translate into far-reaching economic and social losses in countries that are already devastated by war. But it is not just these nations that are affected. Earlier this year, a new strain of monkeypox virus, which causes mpox, rapidly spread among internally displaced people living in camps in Goma, the DRC. These people had fled nearby areas that had been made unsafe by fighting between government forces and militias. Previously, the disease spread mainly through sexual transmission between adults. Now, with the new strain — and probably because of overcrowding and the poor health of people in these camps — children are also being infected, and mortality and morbidity have increased. Indeed, the disease spread so quickly in just three months that in August the WHO designated it as a ‘public health emergency of international concern’.
So how can the international humanitarian community — and global health researchers — better address the health needs of internally displaced people?
Gaining traction
In the past two years, various initiatives have begun to focus more attention on the plight of internally displaced people. In 2022, António Guterres, the UN secretary-general, launched the UN Action Agenda on Internal Displacement, and appointed a special adviser to implement it across the UN system and beyond. Also, a review to identify how the humanitarian system can respond to internal displacement more effectively was commissioned earlier this year by the UN Inter-Agency Standing Committee (IASC), which sets priorities and mobilizes resources in response to humanitarian crises (see go.nature.com/3nx7r5x).
To build on this momentum, we urge the WHO to explicitly address the needs of internally displaced people in its health policies. The organization could draw on the tools it has already been developing to ensure access to health services for other populations that experience hardships disproportionately, for instance because of gender inequalities13.

Millions of people have been internally displaced in the Democratic Republic of the Congo this year.Credit: UNHCR/Guerchom Ndebo
We also urge national governments and international donors to better support the problem; to ensure that resources address the health challenges stemming from internal displacement specifically; and to better monitor the allocation of funds for displacement-affected populations. Efforts must also address health issues for this group of people over the long term — not just in the immediate aftermath of conflict. National efforts to achieve universal health coverage (one of the targets for the UN Sustainable Development Goal to ‘ensure healthy lives and promote well-being for all at all ages’), for example, must take into account the specific needs of internally displaced people.
On the research front, more data on the health of this group of people and their access to health services must be collected. Further research on what is needed to make existing systems responsive to the health needs of this group is also crucial. Since 2021, an independent group of researchers (including the three of us), called the Health and Internal Displacement Network (HIDN), has promoted and conducted research on the health of internally displaced people. Similar initiatives are needed to ensure that medical and health research on a range of diseases adequately addresses the challenges created by internal displacement.
Technological and methodological advances, such as satellite imagery and the use of mobile-phone data, are making it easier for investigators to monitor the movements of groups of people, and to estimate the numbers of people who have been internally displaced or who have lost access to health services and so on14. But, in our view, research efforts will be effective only if displaced people themselves play a central part in data collection, and in the design and monitoring of health services. In Chad and Yemen, community-based data gathering on measures such as mortality is enabling investigators to obtain health data for internally displaced people who are living in dangerous or hard-to-reach rural or urban settings15,16.
End the misery
Obviously, the health problems experienced by internally displaced people cannot be resolved through health-system interventions alone. Ensuring that people are protected from violence and that they have access to clean water, sanitation systems and means of employment is also crucial. This can be achieved through strengthening the broader humanitarian response to internally displaced people — as recommended by this year’s IASC-commissioned review. It can also be achieved by ensuring that efforts to deliver these basic resources are integrated with general work on development to sustain and improve people’s health over the long term.
Governments of countries affected by displacement, providers of international aid and private donors must put an end to the inequity and misery faced by internally displaced people — and ensure that their health is as good as that of the national population.

